Setting Up an MRI Protocol
On this page
Full Protocol Initiation Guide
MRI for Velopharyngeal (VP) imaging has been used routinely and numerous research protocols have been published (Perry & Kuehn, 2007; Perry, 2011; Perry et al., 2012; Perry et al., 2014; Perry, Kuehn, Sutton, & Fang, 2017; Perry, Mason, Sutton, & Kuehn, 2018; Perry et al., 2018; Perry et al., 2019; Haenssler et al., 2020; Pua Schleif et al., 2020; Schenck et al., 2021; Haenssler et al., 2021; Kotlarek et al., 2021; Mason et al., 2021). Our research lab and collaborative partners from the University of Illinois (Dr. Brad Sutton) and Massachusetts General Hospital (Dr. Jonghye Woo) have worked extensively to also develop dynamic MRI methods. These dynamic methods allow for imaging to be obtained up to 166 frames per second (Fu et al., 2017), which allows us to capture natural speech using full sentences. However, these methods are not readily available in most hospital settings. Our current collaborative research is working to develop these technologies to create applications that can be used within the clinical setting (Xing et al., 2021).


In collaboration with Phoenix Children’s Hospital (Dr. Thomas Sitzman) as part of a multi-center clinical trial study, we have successfully established and fully implemented a clinical MRI method to more than 13 hospitals across the US and Canada. The overall goal of this study is to compare the effectiveness of existing surgical procedures for VPI. At the hospitals involved in this NIH funded study, we have established a MRI protocol that uses 3D and 2D sequences to acquire MRI data at rest and during sustained phonation. For more details on VPI-OPS, visit this site.
Child-Friendly Protocol
Our lab has published multiple child-friendly protocols (Kollara & Perry, 2014; Kollara, Perry, & Hudson, 2016; Perry, Juehn, Sutton, & Fang, 2017; Kollara, Schenck, Jaskolka & Perry, 2017; Perry et al., 2018; Perry et al., 2020; Mason et al., 2021) and adaptations (Kotlarek et al., 2021) that allow successful imaging among young children. Our lab has also successfully demonstrated the use of these methods with children as young as 3 years of age; however, children 4 years and older are more likely to have success with these methods. We have successfully imaged over 500 subjects using MRI and have reported success rates among children 4 years and older to be between 97 – 100% (Perry et al., 2019; Kotlarek et al., 2019; Haenssler, Fang, & Perry, 2020) when using these methods. A website was developed by our lab as part of the clinical trial study VPI-OPS and can be used to help train and prepare the child and family.
Some suggestions for ensuring a successful MRI include (see the following references for more details—Kollara & Perry, 2014; Kollara, Schenck, Jaskolka & Perry, 2017; Kotlarek et al., 2021):
- Familiarize the patient with the scanning process
- Allow the patient to explore the MRI machine and scanning room with the parent before the exam
- Describe the MRI scanning experience as a feeling of being in a spaceship to lessen the fear of participating in a medical exam
- Listening to MRI noises through headsets outside the MRI scanning room prior to exam
- Parent present in the scanning groom for the entire duration of the scan
- Investigator communicating with the patient via a speaker-microphone system during the exam
- Frequently checking in with the patient about his/her comfort level
- Small foam cushions/towels placed in the head coil on either side of patient’s head to minimize motion
- Offering blankets to swaddle the child’s arms and legs to limit body motion
- Playing music during static image acquisition to maintain a fixed eye gaze and reduce head motion
Sample Protocols across Different MRI Scanners
There are many published methods for MRI protocols published by our lab (Perry, Kuehn, & Sutton, 2013; Kollara, Schenck, Jaskolka, & Perry; 2017; George et al., 2018; Mason, Riski, Williams, Jones, & Perry, 2021; Perry et al., 2021) & other research labs (Ettema et al., 2002; Narayanan et al., 2004; Beer et al., 2004; Ha, Kuehn, Cohen, & Alperin, 2007; Bae, Kuehn, Conway, & Sutton, 2011; Scott et al., 2014; Sagar & Nimkin, 2015; Pelland et al, 2019) which can be used to establish your site’s MRI protocol. The protocol you use will vary based on the scanner type (Siemens, GE, Phillips) and Tesla strength (1.5 or 3.0T).
MRI Study Protocol—As part of the VPI-OPS study, we have established and successfully implemented a protocol at clinical sites that includes the following sequence of images. In total, the scan time is under 15 minutes but a full 30-minute slot is generally recommended to allow time for the child to slowly acclimate to the MRI.
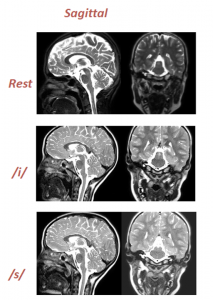
1. 3D static rest in midsagittal
2. 2D static rest in midsagittal
3. 2D static rest in oblique coronal
4. 2D static while the child sustains an “eee” sound in midsagittal
5. 2D static while the child sustains an “eee” sound in oblique coronal
6. 2D static while the child sustains an “sss” sound in midsagittal
7. 2D static while the child sustains an “ssss” sound in oblique coronal
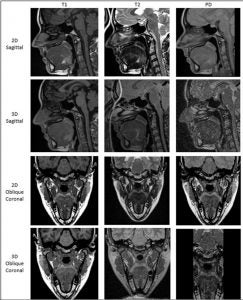
In general, we tend to use T2-Weighted imaging techniques in our lab due to the ability to show the contrast of the muscles. Our methods have been published in numerous journals (Perry, Kuehn & Sutton, 2013; Kollara, Schenck, Jaskolka & Perry, 2017; Fu et al., 2017; Kotlarek et al., 2019; Kollara et al., 2021) and can be applied to any clinical scanner. As seen in the image below, the T2-Weighted produce an image with superior contrast.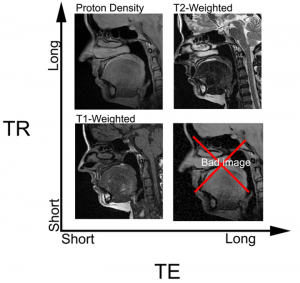
We recently published (Perry et al., 2021) data to suggest that T2-Weighted techniques were rated to produce higher image quality compared to T1 and PD techniques. Additionally, raters rated 2D MRI superior to 3D for image quality but found 3D techniques to be better for identifying key velopharyngeal landmarks. Therefore, we recommend the use of both 3D and 2D and advise hospitals to use their MRI scanner’s pre-set T2-weighted techniques as a starting point.
Critical to a successful MRI is the scan time. Children can only sustain an “ee” or “ss” sound for typically 6-8 seconds. For this reason, any images obtained during speech must be shorter than 8 seconds. Adjusting the TE, TR, FOV, # of slices, etc. are essential steps to shorten the scan time. Publications such as Perry (2011), Perry, Sutton, Kuehn & Gamage (2014), Kollara and Perry (2014), Mason, Pua, and Perry (2018), and Schenck, Perry, Kollara, and Kuehn (2019) demonstrate speech MRI sequences that are within this time frame.
The following references provide additional information to support your site in establishing your VPI MRI protocol:
- Perry, J. L., Sutton, B. P., Kuehn, D. P., & Gamage, J. K. (2014). Using MRI for assessing velopharyngeal structures and function. The Cleft Palate-Craniofacial Journal, 51(4), 476-486.
- Kollara, L., & Perry, J. L. (2014). Effects of gravity on the velopharyngeal structures in children using upright magnetic resonance imaging. The Cleft Palate-Craniofacial Journal, 51(6), 669-676
- Mason, K. N., Riski, J. E., Williams, J. K., Jones, R. A., & Perry, J. L. (2021). Utilization of 3D MRI for the Evaluation of Sphincter Pharyngoplasty Insertion Site in Patients With Velopharyngeal Dysfunction. The Cleft Palate-Craniofacial Journal (in press)
Obtaining the Sagittal and Oblique Coronal Image Planes
There are many image planes that can be obtained using MRI. A description of the anatomy that can be viewed from each image plane is described in the table below.
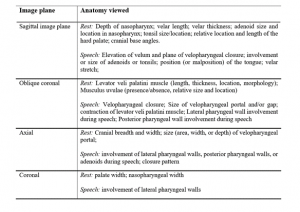
For clinical MRI studies as part of the VPI-OPS, we typically obtain images in the midsagittal and oblique coronal image planes. While the midsagittal image plane is standard in head MRI, an oblique coronal plane is not. The oblique coronal plane, as seen in the table, allows for visualization of the levator veli palatini muscle.
Finding the oblique coronal image plane requires an understanding of the location and direction of the levator veli palatini muscle. In children, this angle is typically between 50-55 degrees and in adults, it is closer to 45 degrees. Setting the angle at this angle should serve as a starting point. Additional guides include the use of the sphenoid-occipital synchondrosis, which is typically in children in the plane of the levator veli palatni muscle. Aligning the oblique coronal with this structural landmark can also provide visualization of the muscle.

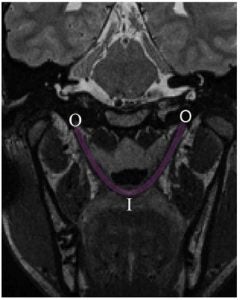
Once an image plane similar to that shown in the above image is achieved, the oblique coronal images obtained should be carefully examined to ensure that the muscle is visible. If it is not visible then the angle should be rotated and images reobtained. This is repeated until the muscle is visible through the origin to the insertion of the muscle. The muscle should appear as seen to the right (Perry, Kuehn, Sutton, 2013).
Eliciting Speech Samples
Eliciting the speech samples can be done by the MRI technologists, child life specialists, or the speech-language pathologist (SLP). If the SLP is available to support the MRI scans, this is the best option because he/she is most aware of the child’s speech abilities. For example, the SLP likely knows if the child is able to even produce the “sss” sound for the scan. If the child is not able to produce this sound because he/she has speech errors still, the SLP can help the child produce a “sh” sound, which can provide valuable insights in place of the “sss” sound. Additionally, the SLP might also be able to cue the child to produce the “sss” as they practice it in speech therapy, thus allowing a more successful speech production. A child life specialist is helpful to prepare the child for the MRI and ensure the child is comfortable, relaxed, and remains still for the exam. This person is often in the room with the child during the MRI study. Whereas the SLP stays in the control room and communicates with the child through the microphone (Kollara & Perry, 2014).
| Keys to Successful Speech Production: |
|---|
| 1. Practice the speech sounds that will be used with the child before the study begins & use this MRI website to prepare the child. When practicing, remind the child to take a breath before the production without moving his/her head. |
| 2. Have a clinician present in the MRI room to ensure that the child’s production was an accurate production of the required speech sound. |
| 3. Instruct the child to produce the “snake sound” as “sssss” and not the letter “s” as “esss.” |
| 4. Begin the scan immediately after you instruct the child to begin the speech production to make sure the sound was sustained for the duration of the scan. |
